When it comes to 3D printing, the sky is the limit. As 3D printing technology continues to advance, applications can be as far reaching as airplane and automobile parts to medical devices and even anatomically correct, biocompatible models. Although 3D printing technology is developing at a rapid pace, the technology itself is not new. It emerged in the 1980s as a means of creating rapid prototypes. In recent years the applications for 3D printed models have evolved with the available hardware, software, and printable materials. Evolving technology, paired with the creative and innovative minds of scientists, engineers, and physicians, has been the launching pad for developments within 3D printing technology specific to healthcare. One way 3D printing technology is poised to create better patient outcomes is in creating an anatomically and patient-specific models to aid in surgery and medical procedures. With the capability to 3D ...
Microprinted artificial cells?
Arrays of them could be used for pharmaceutical testing, targeted drug delivery, gene therapy, and other important biotechnological and medical applications.
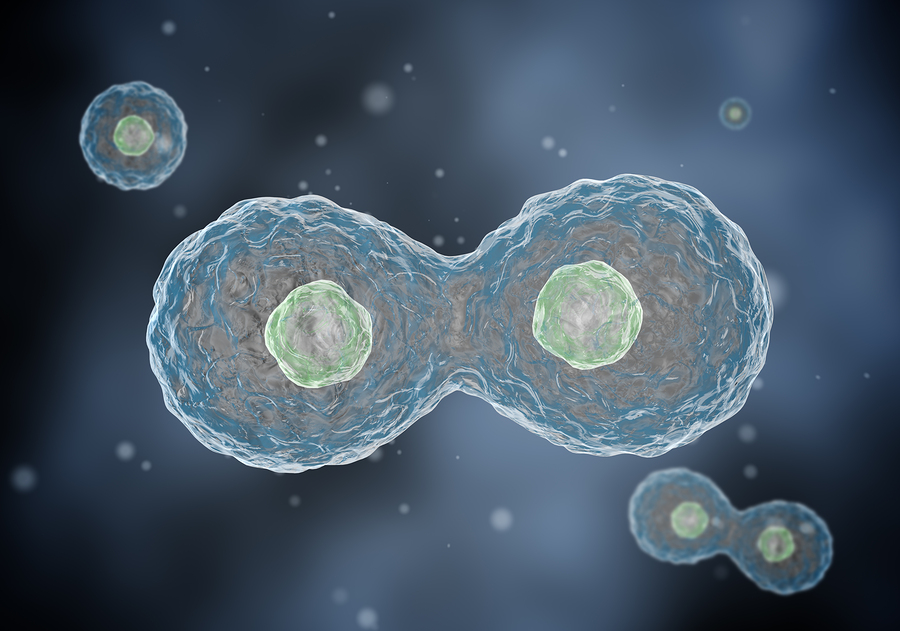
Our knowledge and understanding of cell function is still in its infancy. Attempts to build artificial cells to model cellular transport and processes are currently underway. One of the simplest cell models is a liposome (from the Greek lipo, or fat, and soma, or body), which is a vesicle composed of a lipid bilayer. As seen in the image, the lipids composing the bilayer have hydrophilic heads (facing the aqueous inside and the outside) and hidden hydrophobic tails. Liposomes have many applications, from gene delivery to cosmetics. Larger liposomes (in the range of 1 to 50 microns) — also called “giant unilamellar vesicles,” or GUVs — can incorporate cell membrane proteins and channels, and serve as models for processes in human cells.
When we deal with models, they have to be reproducible. Thus, finding the way to make uniform reproducible GUVs is very important to future studies. A team from Pennsylvania State University made the cover of Advanced Materials in December for having found a way to make arrays of artificial cells using a microprinting approach:
S. Majd and co-workers report a simple approach for the preparation of cell-sized liposomes with integral membrane proteins […] In this approach, hydrogel-stamped lipid/protein deposits grow, upon application of an AC electric field, into giant liposomes of controlled size and composition. The resulting vesicles can be applied in membrane and protein studies, as well as in biotechnology.
Dr. Sheereen Majd, an assistant professor of biomedical engineering, started microprinting lipids years ago. She used agarose, a soft, hydrogel-forming polymer, to make gel stamps for the creation of lipid arrays, used for screening assays of drug–membrane interactions.
Now her group has developed a “simple and versatile method for the formation of arrays of giant vesicles with controlled size and composition.” To make arrays, the mixed proteins and lipids are first applied (or inked) on a structured agarose stamp, then “printed” on a conductive ITO (Indium Tin Oxide) coated glass slide and “grown” in a controlled manner by applying the voltage to the printed electrode.
Recorded using time-lapse fluorescent microscopy, the vesicles grow by bubbling up and merging to form one giant vesicle per application spot, creating an array liposomes the same size. By altering the frequency of the current, the vesicles can be detached from the support, producing a large number of monodisperse giant proteoliposomes. As was featured in Penn State News:
The researchers’ cells […] contain lipids with protein components the way cell membranes exist in nature. The various proteins serve to allow certain materials to enter and leave the cell, acting as regulators […] The variety of lipids and proteins used can vary depending on the ultimate purpose of the artificial cells. The cells that form are between 20 and 50 microns, within the range of natural cells.
The next step will be “to incorporate more than just lipids and proteins into the artificial cells. One possibility is to bind potential drugs to the proteins and lipids.” So in a few years we might have a scalable process for industrial artificial cell production … and why not?
Comments
Post a Comment